papp decryption. Plasma pregnancy-associated protein A (PAPP-A)
Currently, much attention is paid to the early diagnosis of congenital malformations (CM) and hereditary chromosomal diseases. For this, screenings are carried out - mass examinations of all or selected pregnant women according to certain parameters.
information The main goal of the research is the formation of high-risk groups for the birth of children with hereditary pathology for additional tests.
There are the following types of prenatal screening:
- Ultrasound screening. It is carried out without exception for all pregnant women three times: at 10 - 14, 20 - 24 and 32 - 34 weeks of pregnancy.
- Biochemical screening marker proteins in the blood of a pregnant woman. The study is prescribed if there are indications or if any abnormalities were detected during ultrasound. At 10-14 weeks, a “double” test is performed, and at 16-20 weeks, a “triple” test.
- Cytogenetic screening performed by a geneticist. The probability of having a child with a hereditary pathology is calculated based on the family history and the presence of a specific disease in one of the parents. It is most advisable to contact genetics at the stage of pregnancy planning.
- Molecular screening. The DNA of future parents is examined to identify presymptomatic patients and asymptomatic heterozygous carriers of the most common monogenic diseases (cystic fibrosis, phenylketonuria, Duchenne myodystrophy, hemophilia A and B, adrenogenital syndrome, and others). Also carried out before pregnancy.
- Immunological screening. To be carried out by all pregnant women at registration. It includes the determination of Rh and the blood group of both parents and the TORCH complex, infections that potentially disrupt the intrauterine development of the fetus. These include: toxoplasmosis, chickenpox, and herpesvirus infections.
Ultrasound Screening
additionally If any abnormalities are detected, the woman is sent for additional examination to the prenatal diagnostic center or the medical genetic center. Here, a more detailed study of any anatomical disorders is carried out and, together with genetics, pediatricians and pediatric surgeons, the most optimal tactics for further pregnancy management are developed.
On the the second stage of ultrasound (at 20 - 24 weeks of pregnancy) conduct a detailed assessment of the anatomical structures of the fetus to detect malformations, markers of chromosomal pathology, early forms of intrauterine growth retardation, pathology of the placenta and umbilical cord, and an abnormal amount of amniotic fluid. If any violations are detected, then the pregnant woman is also sent to the second and third levels of diagnostics, where functional disorders of the affected organ are studied. Particular attention is paid to anomalies of the heart, brain and placenta. Highly informative is the use of the method of color Doppler mapping.
When conducting third ultrasound (at 32 - 34 weeks) evaluate the growth rate of the fetus, the correspondence of its size to the terms of pregnancy, and also reveal malformations with late manifestation. It is very important in this period to assess the state of blood flow in the mother-placenta-fetus system for early diagnosis and fetal hypoxia. If developmental anomalies are detected at this stage, it is already possible to predict the possibility of surgical correction of the defect and determine the tactics of delivery.
Biochemical screening
Biochemical screening makes it possible to form a high-risk group for the birth of children with congenital malformations and chromosomal diseases. The method is based on the determination of serum markers in the woman's blood. The concentration of these substances changes as the duration of pregnancy increases and if the condition of the fetus is disturbed.
Indications for biochemical screening:
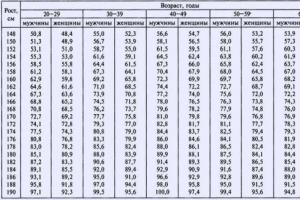
Table: Factors affecting the results of biochemical screening tests:
| Index | Raise | decline |
| Body mass | Reduced | Increased |
| in vitro fertilization | The level of hCG is higher on average by 10 - 15% | Free estriol and PAPP-A levels are about 10 to 20% lower |
| Multiple pregnancy | Most often, the indicators are increased according to the number of fruits 2 | |
| Bleeding threatening miscarriage 1 | AFP | PAPP-A, hCG, free estriol |
| Diabetes | In insulin-dependent diabetes mellitus, the levels of PAPP-A, AFP and free estriol are reduced | |
| Race | AFP and hCG levels are higher in black women compared to Europeans |
To evaluate the "triple" test, the determination of the multiplicity of the median MoM is also used. In various diseases of the fetus, a combined characteristic deviation of biochemical screening indicators is revealed. They are called MoM profiles for a specific pathology. If there are deviations from the norm, first of all, it is necessary to conduct a second ultrasound to clarify the gestational age and identify obvious malformations. If obvious violations are detected, then invasive methods for examining the fetus (chorion biopsy,) are already prescribed to determine the chromosomal set of the fetus.
Description
Method of determination Immunoassay.
Material under study Serum
Home visit available
Pregnancy-associated plasma protein-A. In prenatal screening of the first trimester of pregnancy, it is a marker of the risk of Down syndrome and other fetal chromosomal abnormalities.
PAPP-A is a high molecular weight glycoprotein (m.v. about 800 kDa). During pregnancy, it is produced in large quantities by trophoblasts and enters the maternal circulation system, its concentration in the mother's blood serum increases with increasing gestational age. Based on their biochemical properties, PAPP-A is classified as a metalloprotease. It has the ability to cleave one of the proteins that bind the insulin-like growth factor. This causes an increase in the bioavailability of insulin-like growth factor, which is an important factor in fetal development during pregnancy. It is assumed that PAPP-A is also involved in the modulation of the maternal immune response during pregnancy. A similar protein is also present in low concentrations in the blood of men and non-pregnant women. The physiological role of PAPP-A continues to be explored.
A number of serious clinical studies indicate the diagnostic significance of PAPP-A as a screening marker for the risk of fetal chromosomal abnormalities in early pregnancy (in the first trimester), which is fundamentally important in the diagnosis of chromosomal abnormalities. The level of PAPP-A is significantly reduced if the fetus has trisomy 21 (Down syndrome) or trisomy 18 (Edwards syndrome). In addition, this test is also informative in assessing the threat of miscarriage and termination of pregnancy in the short term.
An isolated study of the level of PAPP-A as a marker of the risk of Down syndrome has diagnostic value, starting from 8-9 weeks of pregnancy. In combination with the determination of beta-hCG (human chorionic gonadotropin), the determination of PAPP-A is optimally carried out at a period of about 12 weeks of pregnancy (11 - 14 weeks). After 14 weeks of gestation, the diagnostic value of PAPP-A as a risk marker for Down syndrome is lost.
It has been established that the combination of this test with the determination of the free beta subunit of hCG (or total beta-hCG), ultrasound data (nuchal thickness), assessment of age-related risk factors significantly increases the effectiveness of prenatal screening for Down syndrome in the first trimester of pregnancy, bringing it to 85 - 90% detection rate of Down syndrome with 5% false positive results. The study of PAPP-A as a biochemical marker of congenital and hereditary pathology in the fetus in combination with the determination of hCG at a period of 11-13 weeks of pregnancy is currently included in the scheme of screening examinations of pregnant women in first trimester.
The detection of deviations in the levels of biochemical markers in the mother's blood is not an unconditional confirmation of fetal pathology, but, in combination with the assessment of other risk factors, it is the basis for the use of more complex special methods for diagnosing fetal anomalies.
Limits of determination: 0.03 mU/ml-100 mU/ml
Training
It is preferable to take blood in the morning on an empty stomach, after 8-14 hours of a night fasting period (you can drink water), it is permissible in the afternoon 4 hours after a light meal.
On the eve of the study, it is necessary to exclude increased psycho-emotional and physical activity (sports training), alcohol intake, an hour before the study - smoking.
Indications for appointment
- Screening examination of pregnant women to assess the risk of fetal chromosomal abnormalities in the 1st and early 2nd trimesters of pregnancy (11-13 weeks).
- Severe complications of pregnancy in history (in order to assess the threat of miscarriage and stop the development of pregnancy in the short term).
- The woman is over 35 years of age.
- The presence of two or more spontaneous abortions in early pregnancy.
- Bacterial and viral (hepatitis, rubella, herpes, cytomegalovirus) infections transferred during the period preceding pregnancy.
- The presence in the family of a child (or in history - the fetus of an interrupted pregnancy) with Down's disease, other chromosomal diseases, congenital malformations.
- Hereditary diseases in close relatives.
- Radiation exposure or other harmful effects on one of the spouses before conception.
The first prenatal screening is a comprehensive study, on the basis of which further pregnancy is predicted, early pathologies and malformations of the fetus are revealed. The examination includes a blood test for the PAPP-A protein. At an early stage of gestation, it is considered one of the important indicators in diagnosing the health of the unborn baby. A pregnancy test for PAPP-A in the first trimester reveals risks, but does not make a diagnosis.
What is RRR-A?
PAPPA-A (pregnancy-associated plasma protein A / pregnancy-associated plasma protein-A) is a macroglobulin, or plasma protein, produced in large quantities by placental fibroblasts during pregnancy. Determined in the bloodstream of the mother. Its concentration increases throughout the entire period of bearing the baby. This protein ensures the full growth and development of the placenta.
An isolated study of PAPPA-A to determine Down's syndrome is possible from 8–9 weeks. But to improve accuracy, it is used in combination with ultrasound (nuchal thickness) and the study of the free beta subunit of hCG (a free unit of human chorionic gonadotropin). Ideally, it is carried out at 12 weeks of gestation (allowable interval: 11 - 14 weeks). The sensitivity and specificity of the combination reaches 95%. Starting from the middle of the second trimester, the diagnostic value of the definition of Down syndrome is not relevant and not informative.
Only the full complex gives a reliable picture of the course of pregnancy. Blood for biochemical screening is donated no later than three days after the ultrasound. These methods are screening, and it is impossible to make a diagnosis with 100% certainty.
If abnormalities are detected, more accurate instrumental studies are prescribed, such as a chorionic villus biopsy (a sample of embryonic tissue is taken by puncturing the abdominal wall with a needle), amniocentesis (puncture of the amniotic membrane and obtaining amniotic fluid), cardiocentesis (blood sampling of an unborn child from the umbilical cord).
Indications for appointment
To take a blood test, you need to contact a gynecologist in the antenatal clinic. Based on the following indications, a test for PAPP-A is prescribed:
- conducting a screening examination of pregnant women at 11-13 weeks;
- complicated pregnancies in history (miscarriages and missed pregnancies);
- age over 35;
- two or more spontaneous abortions;
- bacterial and viral infections that have joined during pregnancy (hepatitis, herpes, CMV, rubella);
- the presence of chromosomal abnormalities in a child;
- heredity (chromosomal abnormalities in the next of kin);
- exposure of one of the spouses to radiation and other types of radiation before conception.

Preparation for blood collection
Proper preparation for the delivery of the analysis leads to a decrease in the likelihood of an erroneous result. After all, the level of indicators is influenced by many factors: body position, food intake, alcohol, drugs and much more.
To get the most correct results, you need to follow certain rules:
- blood is donated on an empty stomach (you need to take food with you to have breakfast after the procedure, water is not prohibited if the patient has toxicosis);
- blood sampling time - from 7.00 to 9.00;
- suitable position - lying;
- the absence of physical activity is important (you need to rest 30 minutes before the office);
- three days before the study, spicy, smoked, fried foods, seafood, nuts, chocolate should be excluded from the diet;
- it is necessary to consult with a doctor about medications that can lead to distortion of the results.
Blood levels
Norms of content in the blood plasma of a pregnant woman PAPP-A, IU / l:
- from the 8th week - 0.18–1.57;
- from the 9th week - 0.33–2.43;
- from the 10th week - 0.47–3.74;
- from the 11th week - 0.80–4.77;
- from the 12th week - 1.04–6.02;
- from the 13th week - 1.48–8.55.
These figures may vary in different laboratories depending on the specificity and sensitivity of the equipment and the method of determination. You should pay attention to the reference values in the test form.
During pregnancy, the level of PAPP-A increases almost a thousand times. After childbirth, macroglobulin decreases sharply in 3-4 days, then decreases by half every subsequent 3 days.
The doctor leading the pregnancy translates the indicators into the MoM coefficient (multiples of median) - this is the percentage of deviation in this woman from the average statistical norm. For calculation, the PAPP-A parameter is divided by the average value corresponding to the week of pregnancy.
Regardless of the laboratory, the IOM coefficient varies from 0.5 to 2.5, with multiple pregnancy it reaches 3.5.
Deciphering the results
If the diagnostic value of PAPP-A is higher than normal, then the possible reasons are:
- multiple pregnancy;
- incorrect determination of gestational age;
- large mass of the placenta;
- large fruit;
- preeclampsia.
Indicators below the norm can talk about the following pathologies and conditions:

It is necessary to seek advice for further monitoring and in the following cases:
- based on the results of screening, the risk is low, but the MoM is less than 0.6 or above 2.0;
- both indicators (MoM and PAPP-A) are below 0.5
This does not mean pregnancy complications, only increases the risk of their occurrence.
With a normal location of the placenta, early labor and fetal malnutrition are observed when there is a low level of PAPP-A in serum at 8–13 weeks.
It has been statistically proven that the concentration of PAPP-A is reduced in women with bleeding at 8–21 weeks of gestation. Almost all patients with low placentation have a small increase in the blood count for the entire pregnancy. If there is a history of diseases such as diabetes mellitus, arterial hypertension, then throughout pregnancy, the concentration of the parameter may be lower. An increase in concentration for a period of 34 weeks is determined in a severe form of late preeclampsia, a precursor of preeclampsia, this is a predictor of bleeding in the postpartum period. Also, in approximately 11% of women whose gestation ended in miscarriage, PAPP-A in the blood serum was elevated.
With a multiple pregnancy, which is included in a number of complicated ones, one embryo can develop normally, and the second one will have signs of pathology that can already be determined at week 12. The result of the test for PAPP-A in any case will be overestimated compared to the established intervals, and this is normal, since the weight of the placenta increases and, accordingly, the production of pregnancy-associated protein increases. In this case, the MOM coefficient, which reaches 3.5, has a diagnostic value.
Features of the PAPP-A results:
- the analysis does not determine the deviation in the development of the neural tube;
- possible 5% false positive result;
- only 2–4% have a chromosomal abnormality;
- not with all anomalies in the fetus, PAPP-A changes.
[08-126 ] Plasma pregnancy-associated protein A (PAPP-A)
820 rub.
Order
It is a protein that is produced in large quantities during pregnancy. According to its level, the risk of chromosomal abnormalities in prenatal diagnosis of fetal pathologies is assessed.
SynonymsEnglish
Pregnancy-associated plasma protein-A (PAPP-A), pappalysin 1.
Research method
Solid-phase chemiluminescent enzyme immunoassay ("sandwich" method).
Units
MME/ml (milli-international unit per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Eliminate fatty foods from the diet for 24 hours before the study.
- Eliminate physical and emotional overstrain and do not smoke 30 minutes before the study.
General information about the study
Pregnancy-associated plasma protein A (PAPP-A) is a zinc-containing enzyme (metalloproteinase). During pregnancy, it is produced in large quantities by fibroblasts in the outer layer of the placenta and decidua and is found in the maternal circulation as a high molecular weight protein fraction.
The PAPP-A enzyme cleaves protein fragments from the insulin-like growth factor and increases its biological activity, which ensures the full growth and development of the placenta. In addition, it is able to inactivate certain enzymes in the blood (trypsin, elastase, plasmin) and modulate the immune response of the mother's body. Its content in the blood increases with the progression of pregnancy. It does not significantly depend on such parameters as the sex and weight of the child. Only during the period of intensive formation of the placenta (7-14 weeks of pregnancy) is there a strong relationship between the level of PAPP-A and the concentration of estradiol. After childbirth, PAPP-A decreases rapidly over several days.
With a chromosomal abnormality with fetal malformations, the concentration of PAPP-A in the blood decreases significantly from the 8th to the 14th week of pregnancy. The most dramatic decrease is noted in trisomy on the 21st, 18th and 13th chromosomes. In Down syndrome, the PAPP-A index is an order of magnitude lower than in the normal. The level of PAPP-A in the mother's blood serum falls even more sharply if the fetus has a genetic pathology with multiple malformations - Cornelia de Lange syndrome.
The test is prescribed in combination with the determination of the beta subunit of chorionic gonadotropin and the study of the thickness of the collar space by ultrasound. This comprehensive examination is recommended for screening for Down syndrome and other fetal chromosomal abnormalities in the first trimester of pregnancy (at 10-13 weeks). A separate determination of PAPP-A is most informative at 8-9 weeks. After 14 weeks of pregnancy, the value of this indicator as a marker of the risk of chromosomal abnormalities is lost, since the level is normal even with pathology.
Based on the results of this test, a decision is made on the advisability of prescribing additional methods for examining the fetus. At the same time, the level of PAPP-A cannot serve as a criterion for making a diagnosis. In normal pregnancies, the test result may be false positive in 5%, and fetal chromosomal abnormalities are detected in only 2-3% of pregnant women with reduced PAPP-A levels. In the United States, the use of this test in the first trimester of pregnancy detects about 85% of cases of Down syndrome and 95% of Edwards syndrome. If the result is positive, additional examinations are necessary, including chorion puncture, amniocentesis with a genetic study of the material obtained.
Minimal amounts of PAPP-A protein can be found in men and non-pregnant women. An increase in PAPP-A is recorded after damage to atherosclerotic plaques in acute coronary syndrome, unstable angina. This protein is being actively studied as a marker for the prognosis of coronary heart disease, but has not yet received wide distribution in cardiac laboratory tests.
What is research used for?
- For screening for possible chromosomal abnormalities in the fetus.
- To assess the threat of premature termination of pregnancy or miscarriage, to predict the course of pregnancy.
When is the study scheduled?
When examining pregnant women in the first trimester (the analysis is recommended at the 10-13th week of pregnancy), especially if there are risk factors for the development of pathology:
- age over 35 years;
- miscarriage and severe complications of pregnancy in the past;
- chromosomal pathologies, Down's disease or congenital malformations in previous pregnancies;
- hereditary diseases in the family;
- past infections, radiation exposure, taking medications in early pregnancy or shortly before it that have a teratogenic effect (can cause birth defects and fetal anomalies).
What do the results mean?
Reference values
Causes of elevated plasma pregnancy-associated protein A (PAPP-A):
- multiple pregnancy,
- large fetus and increased mass of the placenta,
- low placenta.
Causes of low levels of pregnancy-associated plasma protein A (PAPP-A):
- Down syndrome - trisomy on the 21st chromosome (mental retardation, congenital heart disease, characteristic facial features and other anomalies);
- Edwards syndrome - trisomy on the 18th chromosome (profound mental retardation, heart defects, anomalies in the structure of the skull, low ears, dysplasia of the feet and other anomalies);
- Patau syndrome - trisomy on the 13th chromosome (cleft lip and palate, polydactyly - extra fingers or toes, underdevelopment of the external genitalia, microcephaly - reduced size of the skull and brain, microphthalmia - underdevelopment of the eye, and other anomalies);
- Cornelia de Lange syndrome - a genetic disease with multiple congenital malformations (stunted growth and development, mental retardation, microcephaly, visual impairment, splitting of the hard palate and other anomalies);
- the threat of miscarriage and early termination of pregnancy;
- fetoplacental insufficiency;
- fetal malnutrition (insufficient weight due to malnutrition).
What can influence the result?
- With multiple pregnancies, the content of PAPP-A in the mother's blood increases and it is difficult to assess the likelihood of chromosomal abnormalities.
- If the gestational age of the fetus is incorrectly determined, the result may be falsely increased or decreased.
Important Notes
- The test for pregnancy-associated plasma protein A in pregnant women is not used to diagnose fetal pathology and placental insufficiency, but to assess their likelihood. Making a decision to terminate a pregnancy based on changes in PAPP-A levels would be a big mistake.
- The use of invasive diagnostic methods (chorionic biopsy, amniocentesis, cordocentesis) is not recommended if screening tests are normal and there are no changes on ultrasound.
- Placental lactogen
Who orders the study?
Obstetrician-gynecologist, medical geneticist.
Literature
- Gorin V. S., Serov V. N. and others . Pregnancy-associated protein A and other macroglobulins as protein markers of perinatal pathology. Russian Bulletin of Perinatology and Pediatrics, N 4, 1998, pp. 18-24.
- Body R., Ferguson C. Pregnancy associated plasma protein A: a novel cardiac marker with promise. Emerge Med J. 2006 November; 23(11): 875–877. PMCID: PMC2464389.
- Brügger-Andersen T, Bostad L, and others. The activity of pregnancy-associated plasma protein A (PAPP-A) as expressed by immunohistochemistry in atherothrombotic plaques obtained by aspiration thrombectomy in patients presenting with a ST-elevation myocardial infarction: a brief communication. Thromb J. 2010 Jan 27;8(1):1. PMID: 20181026 .
Opinions about the information content of prenatal screenings differ. Some believe that this is another reason to worry. Others are convinced that the analysis can serve as the first signal of a real threat. However, it is still better to play it safe, especially in those matters that relate to the health of the unborn baby. In particular, the analysis of Papp-A during pregnancy (the Russian-language version of Papp-A), which is carried out during pregnancy, will help clarify the picture.
Analysis of Papp-A (Papp-A) during pregnancy - what is the point?
A characteristic marker of the risk of having a child with some problems at the gene level is the level of Papp-A during pregnancy, or more precisely, its compliance with the norm. If we literally decipher and translate this abbreviation from English, then Papp-A turns out to be nothing more than the A-plasma protein associated with pregnancy, the concentration of which increases in proportion to the period.
Doctors recommend to be examined from 8 to 14 weeks of pregnancy. But, since Papp-A is determined in combination with hCG, the optimal time for taking the Papp-A analysis during pregnancy is the interval from 11 to 13 weeks. At this stage, the results obtained will be as informative as possible.
Because Papp-A can indicate fetal chromosomal abnormalities, a double test is strongly recommended for women:
- over the age of 35;
- already having children with similar problems;
- having relatives with genetic disorders;
- who had been ill with rubella, hepatitis, or herpes shortly before pregnancy;
- with complicated or interrupted pregnancies in the early stages, in the past.
If Papp-A does not meet the norm during pregnancy, the doctor will prescribe an additional examination in order to make sure that everything is fine with the baby.
The unit of measurement of Papp-A is m U / ml, and the limits of the norm depend on the gestational age, thus:
- 0.17-1.54 range of acceptable values for a period of 8-9 weeks;
- 0,32-2,2 – 9-10;
- 0,46-3,73 – 10-11;
- 0,79-4,76 – 11-12;
- 1,03-6,01 – 12-13.
Reduced and elevated Papp-A (Papp-A) during pregnancy
 If the analysis for Papp-A (Papp-A) during pregnancy has a low content of this protein in the mother's body, this may indicate the likelihood of some chromosomal abnormalities. Also, an underestimated value may indicate a threat of miscarriage or missed pregnancy.
If the analysis for Papp-A (Papp-A) during pregnancy has a low content of this protein in the mother's body, this may indicate the likelihood of some chromosomal abnormalities. Also, an underestimated value may indicate a threat of miscarriage or missed pregnancy.
If Papp-A is elevated during pregnancy, then most likely there was an error in determining the gestational age itself. Therefore, experts recommend that before doing screening, first undergo an ultrasound scan to determine the exact gestational age. At the same time, an increased value does not exclude the possibility of the presence of pathological disorders.